Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- No More NAFLD: The Term Is Now MASLD
- Ji Cheol Bae
- Endocrinol Metab. 2024;39(1):92-94. Published online February 13, 2024
- DOI: https://doi.org/10.3803/EnM.2024.103
- 1,099 View
- 62 Download

- Diabetes, obesity and metabolism
- Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
- Eunju Yoon, Ji Cheol Bae, Sunghwan Suh
- Endocrinol Metab. 2023;38(5):538-544. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1730
- 1,931 View
- 110 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Despite the well-recognized health benefits of fresh fruit consumption, there is still substantial uncertainty about its potential effects on glycemic control in patients with type 2 diabetes mellitus (T2DM).
Methods
We examined the association of fresh fruit consumption and glycemic control in patients with T2DM using data from the 6th Korea National Health and Nutrition Examination Survey. The study sample was divided into three groups based on weekly fruit consumption frequency for the analysis.
Results
Patients with the highest fruit intake were older than those in the other two groups, and women were more likely to consume fruits in general. Being a current smoker and weekly alcohol intake also showed negative correlations according to the fruit intake tertiles. Fruit consumption was positively correlated with better hemoglobin A1c (HbA1c) levels. Moreover, patients in the highest tertile of fruit intake were 3.48 times more likely to be in good glycemic control defined as HbA1c <7%.
Conclusion
We observed that fruit consumption can be helpful in glycemic control in Korean patients with T2DM. -
Citations
Citations to this article as recorded by- The Relationship between Alcohol Consumption and Diabetes in Korean Adults
Gi Tae Kim, Jae Woong Sull
Biomedical Science Letters.2023; 29(3): 159. CrossRef
- The Relationship between Alcohol Consumption and Diabetes in Korean Adults

- Diabetes, obesity and metabolism
- Greater Severity of Steatosis Is Associated with a Higher Risk of Incident Diabetes: A Retrospective Longitudinal Study
- Ji Min Han, Jung Hwan Cho, Hye In Kim, Sunghwan Suh, Yu-Ji Lee, Jung Won Lee, Kwang Min Kim, Ji Cheol Bae
- Endocrinol Metab. 2023;38(4):418-425. Published online July 12, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1729
- 1,056 View
- 77 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Fatty liver is associated with increased risk of developing type 2 diabetes. We aimed to evaluate whether the severity of hepatic steatosis is associated with incident diabetes.
Methods
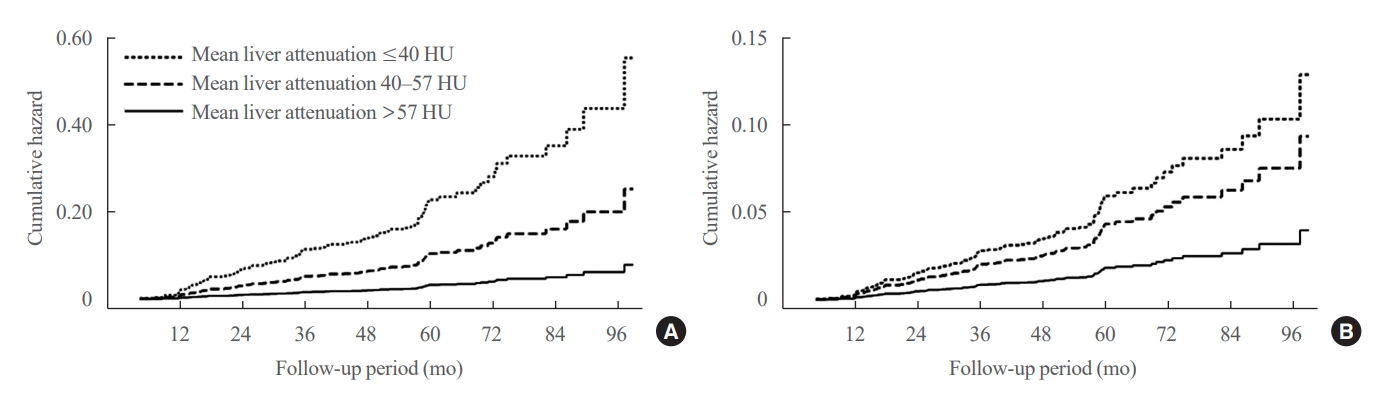
We conducted a longitudinal analysis using data from 1,798 participants who underwent a comprehensive health checkup and abdominal computed tomography (CT). We assessed the association between baseline liver attenuation value on non-contrast CT images and risk of incident diabetes. All the participants were categorized into three groups based on the baseline liver attenuation value on non-contrast CT images: without hepatic steatosis (>57 Hounsfield unit [HU]), mild hepatic steatosis (41–57 HU), and moderate to severe hepatic steatosis (≤40 HU).
Results
During a median follow-up period of 5 years, 6.0% of the study participants progressed to diabetes. The incidence of diabetes was 17.3% in the moderate to severe hepatic steatosis group, 9.0% in the mild steatosis group, and 2.9% in those without hepatic steatosis. In a multivariate adjustment model, as compared with participants without hepatic steatosis, those with moderate to severe steatosis had a hazard ratio (HR) of 3.24 (95% confidence interval [CI], 1.64 to 4.2) for the development of diabetes, and those in the mild steatosis group had a HR of 2.33 (95% CI, 1.42 to 3.80). One standard deviation decrease in mean CT attenuation values of the liver was associated with a 40% increase in the development of diabetes (multivariate adjusted HR, 1.40; 95% CI, 1.2 to 1.63).
Conclusion
We found a positive association between severity of hepatic steatosis and risk of incident diabetes. Greater severity of steatosis was associated with a higher risk of incident diabetes.

- Diabetes, Obesity and Metabolism
- DPP-4 Inhibitor in Type 2 Diabetes Mellitus Patient with Non-Alcoholic Fatty Liver Disease: Achieving Two Goals at Once?
- Ji Cheol Bae
- Endocrinol Metab. 2022;37(6):858-860. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.605
- 1,922 View
- 206 Download
- 4 Web of Science
- 4 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Vildagliptin inhibits high fat and fetuin-A mediated DPP-4 expression, intracellular lipid accumulation and improves insulin secretory defects in pancreatic beta cells
Snehasish Nag, Samanwita Mandal, Oindrila Mukherjee, Tanmay Majumdar, Satinath Mukhopadhyay, Rakesh Kundu
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2024; 1870(3): 167047. CrossRef - Physiology, pharmacology and prospects for dipeptidilpeptidase-4 inhibitors use
D. V. Kurkin, D. A. Bakulin, E. I. Morkovin, A. V. Strygin, Yu. V. Gorbunova, E. V. Volotova, I. E. Makarenko, V. B. Saparova, R. V. Drai, V. I. Petrov
Pharmacy & Pharmacology.2023; 11(1): 19. CrossRef - Comparative effects between old and new antidiabetic agents on metabolic- associated fatty liver disease (MAFLD)
André J. Scheen
Diabetes Epidemiology and Management.2023; 11: 100145. CrossRef - Pharmacokinetic, toxicological, and clinical considerations for the treatment of type 2 diabetes in patients with liver disease: a comprehensive update
André J. Scheen
Expert Opinion on Drug Metabolism & Toxicology.2023; 19(8): 543. CrossRef
- Vildagliptin inhibits high fat and fetuin-A mediated DPP-4 expression, intracellular lipid accumulation and improves insulin secretory defects in pancreatic beta cells

- Diabetes, Obesity and Metabolism
- The Impact of Insulin Resistance on Hepatic Fibrosis among United States Adults with Non-Alcoholic Fatty Liver Disease: NHANES 2017 to 2018
- Ji Cheol Bae, Lauren A. Beste, Kristina M. Utzschneider
- Endocrinol Metab. 2022;37(3):455-465. Published online June 21, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1434
- 4,202 View
- 135 Download
- 9 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We aimed to investigate the association of hepatic steatosis with liver fibrosis and to assess the interactive effects of hepatic steatosis and insulin resistance on liver fibrosis in a nationally representative sample of United States adults.
Methods
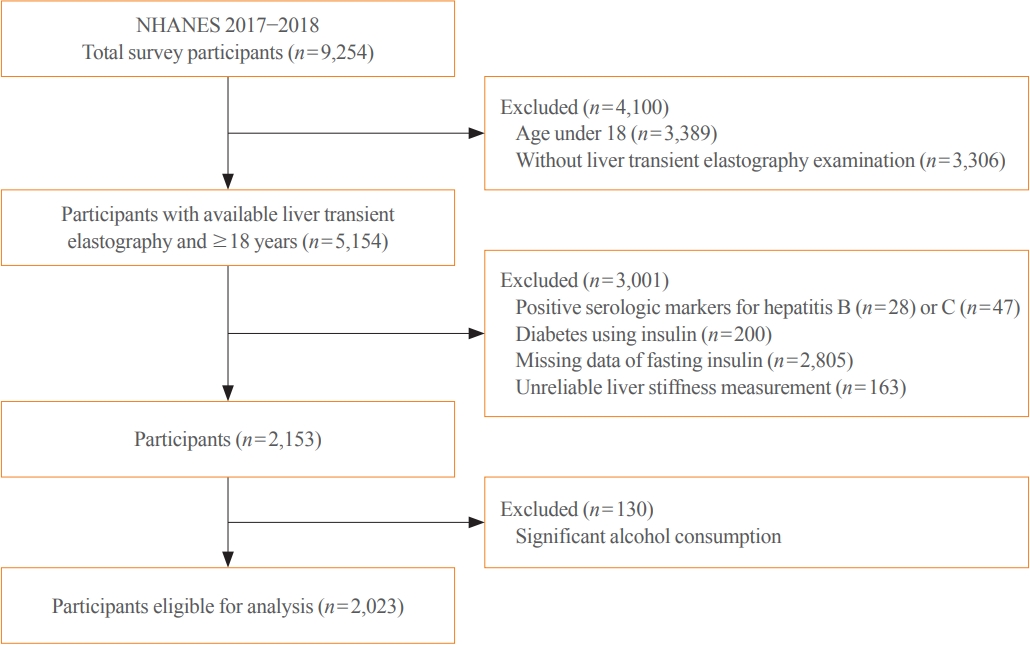
We conducted a cross-sectional analysis using data from National Health and Nutrition Examination Survey 2017 to 2018, which for the first time included transient elastography to assess liver stiffness and hepatic steatosis. We evaluated the association between hepatic steatosis (using controlled attenuation parameter [CAP]) and clinically significant liver fibrosis (defined as liver stiffness ≥7.5 kPa) using logistic regression with an interaction term for hepatic steatosis and insulin resistance (defined as homeostatic model assessment of insulin resistance ≥3.0).
Results
Among adults undergoing transient elastography (n=2,023), 45.9% had moderate or greater hepatic steatosis and 11.3% had clinically significant liver fibrosis. After adjustment for demographic and metabolic factors, the odds of significant liver fibrosis increased as CAP score rose (odds ratio, 1.35 per standard deviation increment; 95% confidence interval, 1.11 to 1.64). We detected a significant interaction effect between CAP score and insulin resistance on the probability of significant liver fibrosis (P=0.016 for interaction). The probability of significant liver fibrosis increased in the presence of insulin resistance with increasing CAP score, while those without insulin resistance had low probability of significant liver fibrosis, even with high CAP scores.
Conclusion
Individuals with hepatic steatosis had higher odds of fibrosis when insulin resistance was present. Our findings emphasize the importance of the metabolic aspects of the disease on fibrosis risk and suggest a need to better identify patients with metabolic associated fatty liver disease. -
Citations
Citations to this article as recorded by- Association of insulin resistance indicators with hepatic steatosis and fibrosis in patients with metabolic syndrome
Tzu-chia Kuo, Yang-bor Lu, Chieh-lun Yang, Bin Wang, Lin-xin Chen, Ching-ping Su
BMC Gastroenterology.2024;[Epub] CrossRef - No More NAFLD: The Term Is Now MASLD
Ji Cheol Bae
Endocrinology and Metabolism.2024; 39(1): 92. CrossRef - Insulin Resistance/Sensitivity Measures as Screening Indicators of Metabolic-Associated Fatty Liver Disease and Liver Fibrosis
Mohammad E. Khamseh, Mojtaba Malek, Soodeh Jahangiri, Sohrab Nobarani, Azita Hekmatdoost, Marieh Salavatizadeh, Samira Soltanieh, Haleh Chehrehgosha, Hoda Taheri, Zeinab Montazeri, Fereshteh Attaran, Faramarz Ismail-Beigi, Fariba Alaei-Shahmiri
Digestive Diseases and Sciences.2024;[Epub] CrossRef - The association of Neuromedin U levels and non-alcoholic fatty liver disease: A comparative analysis
Murat Keskin, Sercan Avul, Aylin Beyaz, Nizameddin Koca
Heliyon.2024; 10(5): e27291. CrossRef - Oral Insulin Alleviates Liver Fibrosis and Reduces Liver Steatosis in Patients With Metabolic Dysfunction-associated Steatohepatitis and Type 2 Diabetes: Results of Phase II Randomized, Placebo-controlled Feasibility Clinical Trial
Yuval Ishay, Joel Neutel, Yotam Kolben, Ram Gelman, Orly Sneh Arbib, Oliver Lopez, Helena Katchman, Rizwana Mohseni, Miriam Kidron, Yaron Ilan
Gastro Hep Advances.2024; 3(3): 417. CrossRef - Comparative and Predictive Significance of Serum Leptin Levels in Non-alcoholic Fatty Liver Disease
Mehwish Qamar, Abeer Fatima, Ambreen Tauseef, Muhammad I Yousufzai, Ibrahim Liaqat, Qanbar Naqvi
Cureus.2024;[Epub] CrossRef - Greater Severity of Steatosis Is Associated with a Higher Risk of Incident Diabetes: A Retrospective Longitudinal Study
Ji Min Han, Jung Hwan Cho, Hye In Kim, Sunghwan Suh, Yu-Ji Lee, Jung Won Lee, Kwang Min Kim, Ji Cheol Bae
Endocrinology and Metabolism.2023; 38(4): 418. CrossRef - Hepatic T-cell senescence and exhaustion are implicated in the progression of fatty liver disease in patients with type 2 diabetes and mouse model with nonalcoholic steatohepatitis
Byeong Chang Sim, Yea Eun Kang, Sun Kyoung You, Seong Eun Lee, Ha Thi Nga, Ho Yeop Lee, Thi Linh Nguyen, Ji Sun Moon, Jingwen Tian, Hyo Ju Jang, Jeong Eun Lee, Hyon-Seung Yi
Cell Death & Disease.2023;[Epub] CrossRef - Familial clustering of nonalcoholic fatty liver disease in first‐degree relatives of adults with lean nonalcoholic fatty liver disease
Sorachat Niltwat, Chanin Limwongse, Natthinee Charatcharoenwitthaya, Duangkamon Bunditvorapoom, Wimolrak Bandidniyamanon, Phunchai Charatcharoenwitthaya
Liver International.2023; 43(12): 2713. CrossRef - Metabolic Score for Insulin Resistance Is Inversely Related to Incident Advanced Liver Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease
Jun-Hyuk Lee, Yu-Jin Kwon, Kyongmin Park, Hye Sun Lee, Hoon-Ki Park, Jee Hye Han, Sang Bong Ahn
Nutrients.2022; 14(15): 3039. CrossRef - DPP-4 Inhibitor in Type 2 Diabetes Mellitus Patient with Non-Alcoholic Fatty Liver Disease: Achieving Two Goals at Once?
Ji Cheol Bae
Endocrinology and Metabolism.2022; 37(6): 858. CrossRef
- Association of insulin resistance indicators with hepatic steatosis and fibrosis in patients with metabolic syndrome

- Clinical Study
- Association of Body Mass Index with the Risk of Incident Type 2 Diabetes, Cardiovascular Disease, and All-Cause Mortality: A Community-Based Prospective Study
- Ji Cheol Bae, Nam H. Cho, Jae Hyeon Kim, Kyu Yeon Hur, Sang-Man Jin, Moon-Kyu Lee
- Endocrinol Metab. 2020;35(2):416-424. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.416

- 8,116 View
- 156 Download
- 13 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 2 diabetes and cardiovascular disease (CVD) are the most important sequelae of obesity and the leading cause of death. We evaluated the association between body mass index (BMI) and the risk of incident type 2 diabetes, CVD, and all-cause mortality in a prospective study of a Korean population.
Methods
The shapes of the associations were modeled by restricted cubic splines regression analysis. After categorizing all subjects (n=8,900) into octiles based on their BMI levels, we estimated the hazard ratio (HR) for the association of categorized BMI levels with the risk of incident CVD and type 2 diabetes using a Cox’s proportional hazard analysis.
Results
The mean age of participants was 52 years and 48% were men. Of the subjects at baseline, 39.0% of men and 45.6% of women were classified as obese (BMI ≥25 kg/m2). Over a mean follow-up of 8.1 years, CVD events occurred in 509 participants; 436 died; and 1,258 subjects developed type 2 diabetes. The increased risk of incident diabetes began to be significant at BMI 23 to 24 kg/m2 in both sexes (HR, 1.8). For CVD events, the risk began to increase significantly at BMI 26 to 28 kg/m2 (HR, 1.6). We found a reverse J-shaped relationship between BMI and all-cause mortality, with an increased risk among individuals with BMI values in lower range (BMI <21 kg/m2).
Conclusion
These results suggest that the BMI cut-off points for observed risk were varied depending on the diseases and that the BMI classification of obesity need to be revised to reflect differential risk of obesity-related diseases. -
Citations
Citations to this article as recorded by- Association of obesity with cardiovascular disease in the absence of traditional risk factors
Hui Luo, Yesong Liu, Xue Tian, Yuhan Zhao, Lulu Liu, Zemeng Zhao, Lili Luo, Yanmin Zhang, Xiaozhong Jiang, Yeqiang Liu, Yanxia Luo, Anxin Wang
International Journal of Obesity.2024; 48(2): 263. CrossRef - Clinical characteristics and degree of cardiovascular risk factor control in patients with newly-diagnosed type 2 diabetes in Catalonia
Anna Ramírez-Morros, Josep Franch-Nadal, Jordi Real, Queralt Miró-Catalina, Magdalena Bundó, Bogdan Vlacho, Didac Mauricio
Frontiers in Endocrinology.2024;[Epub] CrossRef - Metabolic status indicators and influencing factors in non-obese, non-centrally obese nonalcoholic fatty liver disease
Zhipeng Huang, Donghong Wei, Xueping Yu, Zicheng Huang, Yijie Lin, Wenji Lin, Zhijun Su, Jianjia Jiang
Medicine.2023; 102(6): e32922. CrossRef - Establishment and health management application of a prediction model for high-risk complication combination of type 2 diabetes mellitus based on data mining
Xin Luo, Jijia Sun, Hong Pan, Dian Zhou, Ping Huang, Jingjing Tang, Rong Shi, Hong Ye, Ying Zhao, An Zhang, Yee Gary Ang
PLOS ONE.2023; 18(8): e0289749. CrossRef - Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2023; 47(6): 846. CrossRef - Relationship between advanced lung cancer inflammation index and long-term all-cause, cardiovascular, and cancer mortality among type 2 diabetes mellitus patients: NHANES, 1999–2018
Yaying Chen, Mengqian Guan, Ruiqi Wang, Xuewen Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Body mass index at baseline directly predicts new-onset diabetes and to a lesser extent incident cardio-cerebrovascular events, but has a J-shaped relationship to all-cause mortality
Yoon-Jong Bae, Sang-Jun Shin, Hee-Taik Kang
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association of Shift Work with Normal-Weight Obesity in Community-Dwelling Adults
Chul Woo Ahn, Sungjae Shin, Seunghyun Lee, Hye-Sun Park, Namki Hong, Yumie Rhee
Endocrinology and Metabolism.2022; 37(5): 781. CrossRef - The Prognostic Value of Combined Status of Body Mass Index and Psychological Well-Being for the Estimation of All-Cause and CVD Mortality Risk: Results from a Long-Term Cohort Study in Lithuania
Dalia Lukšienė, Abdonas Tamosiunas, Ricardas Radisauskas, Martin Bobak
Medicina.2022; 58(11): 1591. CrossRef - The Relationship between Body Mass Index and Incident Diabetes Mellitus in Chinese Aged Population: A Cohort Study
M. L. Tang, Y. Q. Zhou, A. Q. Song, J. L. Wang, Y. P. Wan, R. Y. Xu, Carol Forsblom
Journal of Diabetes Research.2021; 2021: 1. CrossRef - Correlation between adiponectin level and the degree of fibrosis in patients with non-alcoholic fatty liver disease
Manal Sabry Mohamed, Tarek Mohammed Youssef, Esraa Ebrahim Abdullah, Ahmed Elmetwally Ahmed
Egyptian Liver Journal.2021;[Epub] CrossRef - Obesity Measures as Predictors of Type 2 Diabetes and Cardiovascular Diseases among the Jordanian Population: A Cross-Sectional Study
Hana Alkhalidy, Aliaa Orabi, Khadeejah Alnaser, Islam Al-Shami, Tamara Alzboun, Mohammad D. Obeidat, Dongmin Liu
International Journal of Environmental Research and Public Health.2021; 18(22): 12187. CrossRef
- Association of obesity with cardiovascular disease in the absence of traditional risk factors

- Thyroid
- Clinical Outcomes of Differentiated Thyroid Cancer Patients with Local Recurrence or Distant Metastasis Detected in Old Age
- Ji Min Han, Ji Cheol Bae, Hye In Kim, Sam Kwon, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
- Endocrinol Metab. 2018;33(4):459-465. Published online November 30, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.4.459
- 4,760 View
- 54 Download
- 5 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Differentiated thyroid carcinoma (DTC) shows a very good prognosis, but older patients have a higher recurrence rate and those show poor prognosis than younger patients. The aim of this study was to determine the clinical outcomes of thyroid cancer patients who experienced recurrence in old age according to the treatment strategy used.
Methods This retrospective observational cohort study was conducted at Asan Medical Center, Seoul, Korea. Among DTC patients with no evidence of disease after initial treatment, we enrolled 86 patients who experienced recurrence at an age >65 years from 1994 to 2012. Sixty-nine patients had local recurrence and 17 patients showed distant metastasis.
Results The mean age of patients at recurrence was 72 years. Patients were followed up for a median of 4.1 years after recurrence. Sixty-three of the 69 patients with local recurrence received additional treatment, while the other six received conservative care. The cancer-specific mortality rate was 15.5% in the local recurrence group. Airway problems were the main cause of death in patients who did not receive further treatment for local recurrence. Among the 17 patients with distant metastasis, 10 underwent specific treatment for metastasis and seven received only supportive management. Seven of those 17 patients died, and the cancer-specific mortality rate was 35% in the distant metastasis group.
Conclusion The overall cancer-specific mortality rate was 20% in DTC patients in whom recurrence was first detected at an age >65 years. Mortality due to uncontrolled local disease occurred frequently in patients who did not receive definitive management for recurrence.
-
Citations
Citations to this article as recorded by- Identification of Circulating Tumor Cell Phenotype in Differentiated Thyroid Carcinoma
Huiling Wang, Mian Lv, Yonghong Huang, Xiaoming Pan, Changyuan Wei
Journal of Biomaterials and Tissue Engineering.2022; 12(4): 813. CrossRef - Long-Term Outcomes and Prognoses of Elderly Patients (≥65-Years-Old) With Distant Metastases From Well-Differentiated Thyroid Cancer During Radioiodine Therapy and Follow-Up
Zhong-Ling Qiu, Chen-Tian Shen, Zhen-Kui Sun, Hong-Jun Song, Chuang Xi, Guo-Qiang Zhang, Yang Wang, Quan-Yong Luo
Frontiers in Endocrinology.2021;[Epub] CrossRef - Head-to-Head Comparison of Neck 18F-FDG PET/MR and PET/CT in the Diagnosis of Differentiated Thyroid Carcinoma Patients after Comprehensive Treatment
Yangmeihui Song, Fang Liu, Weiwei Ruan, Fan Hu, Muhsin H. Younis, Zairong Gao, Jie Ming, Tao Huang, Weibo Cai, Xiaoli Lan
Cancers.2021; 13(14): 3436. CrossRef - Highly sensitive electrochemical immunosensor using a protein-polyvinylidene fluoride nanocomposite for human thyroglobulin
Maria Oneide Silva de Moraes, João de Deus Pereira de Moraes Segundo, Marcos Marques da Silva Paula, Maria Goreti Ferreira Sales, Walter Ricardo Brito
Bioelectrochemistry.2021; 142: 107888. CrossRef
- Identification of Circulating Tumor Cell Phenotype in Differentiated Thyroid Carcinoma

- Obesity and Metabolism
- Klinefelter Syndrome and Metabolic Disorder
- Ji Cheol Bae
- Endocrinol Metab. 2016;31(4):535-536. Published online December 20, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.535
- 2,862 View
- 33 Download
- 1 Web of Science
- 1 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Epicardial fat: the role of testosterone and lipid metabolism in a cohort of patients with Klinefelter syndrome
S. Granato, G. Barbaro, M.R. Di Giorgio, F.M. Rossi, C. Marzano, F. Impronta, M. Spaziani, A. Anzuini, A. Lenzi, A.F. Radicioni
Metabolism.2019; 95: 21. CrossRef
- Epicardial fat: the role of testosterone and lipid metabolism in a cohort of patients with Klinefelter syndrome

- Obesity and Metabolism
- Diabetes Drugs and Cardiovascular Safety
- Ji Cheol Bae
- Endocrinol Metab. 2016;31(2):239-244. Published online June 10, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.239
- 3,614 View
- 38 Download
- 15 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Diabetes is a well-known risk factor of cardiovascular morbidity and mortality, and the beneficial effect of improved glycemic control on cardiovascular complications has been well established. However, the rosiglitazone experience aroused awareness of potential cardiovascular risk associated with diabetes drugs and prompted the U.S. Food and Drug Administration to issue new guidelines about cardiovascular risk. Through postmarketing cardiovascular safety trials, some drugs demonstrated cardiovascular benefits, while some antidiabetic drugs raised concern about a possible increased cardiovascular risk associated with drug use. With the development of new classes of drugs, treatment options became wider and the complexity of glycemic management in type 2 diabetes has increased. When choosing the appropriate treatment strategy for patients with type 2 diabetes at high cardiovascular risk, not only the glucose-lowering effects, but also overall benefits and risks for cardiovascular disease should be taken into consideration.
-
Citations
Citations to this article as recorded by- Dipeptidyl peptidase-4 inhibitor compared with sulfonylurea in combination with metformin: cardiovascular and renal outcomes in a propensity-matched cohort study
Kyoung Jin Kim, Jimi Choi, Juneyoung Lee, Jae Hyun Bae, Jee Hyun An, Hee Young Kim, Hye Jin Yoo, Ji A. Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Cardiovascular Diabetology.2019;[Epub] CrossRef - Sodium‐glucose cotransporter 2 inhibitors regulate ketone body metabolism via inter‐organ crosstalk
Jin Hee Kim, Minyoung Lee, Soo Hyun Kim, So Ra Kim, Byung‐Wan Lee, Eun Seok Kang, Bong‐Soo Cha, Jin Won Cho, Yong‐ho Lee
Diabetes, Obesity and Metabolism.2019; 21(4): 801. CrossRef - Glitazones and alpha-glucosidase inhibitors as the second-line oral anti-diabetic agents added to metformin reduce cardiovascular risk in Type 2 diabetes patients: a nationwide cohort observational study
Cheng-Wei Chan, Chu-Leng Yu, Jiunn-Cherng Lin, Yu-Cheng Hsieh, Che-Chen Lin, Chen-Ying Hung, Cheng-Hung Li, Ying-Chieh Liao, Chu-Pin Lo, Jin-Long Huang, Ching-Heng Lin, Tsu-Juey Wu
Cardiovascular Diabetology.2018;[Epub] CrossRef - Normoglucemiantes orales y riesgo cardiovascular
Guillermo Guzmán, Juan Esteban Gómez, Leidy Johanna Plaza, María Claudia Sánchez
Revista Colombiana de Cardiología.2018; 25(5): 333. CrossRef - Dipeptidyl peptidase-4 inhibitor use and risk of diabetic retinopathy: A population-based study
N.H. Kim, J. Choi, N.H. Kim, K.M. Choi, S.H. Baik, J. Lee, S.G. Kim
Diabetes & Metabolism.2018; 44(4): 361. CrossRef - Obesity and Type 2 Diabetes in Our Youth: A Recipe for Cardiovascular Disease
Angela Kaye Wooton, Lynne M. Melchior
The Journal for Nurse Practitioners.2017; 13(3): 222. CrossRef - Sex-gender-related therapeutic approaches for cardiovascular complications associated with diabetes
Ilaria Campesi, Flavia Franconi, Giuseppe Seghieri, Marco Meloni
Pharmacological Research.2017; 119: 195. CrossRef - The Landscape of Glucose-Lowering Therapy and Cardiovascular Outcomes: From Barren Land to Metropolis
Mona P. Nasrallah, Charbel Abi Khalil, Marwan M. Refaat
BioMed Research International.2017; 2017: 1. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- Dipeptidyl peptidase-4 inhibitor compared with sulfonylurea in combination with metformin: cardiovascular and renal outcomes in a propensity-matched cohort study

- Clinical Study
- Triiodothyronine Levels Are Independently Associated with Metabolic Syndrome in Euthyroid Middle-Aged Subjects
- Hye Jeong Kim, Ji Cheol Bae, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh, Myung Hi Yoo, Jae Hyeon Kim, Yong-Ki Min, Sun Wook Kim, Jae Hoon Chung
- Endocrinol Metab. 2016;31(2):311-319. Published online May 13, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.311
- 4,454 View
- 32 Download
- 26 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Recent studies have shown an association between thyroid hormone levels and metabolic syndrome (MetS) among euthyroid individuals; however, there have been some inconsistencies between studies. Here, we evaluated the relationship between thyroid hormone levels and MetS in euthyroid middle-aged subjects in a large cohort.
Methods A retrospective analysis of 13,496 euthyroid middle-aged subjects who participated in comprehensive health examinations was performed. Subjects were grouped according to thyroid stimulating hormone, total triiodothyronine (T3), total thyroxine (T4), and T3-to-T4 ratio quartile categories. We estimated the odds ratios (ORs) for MetS according to thyroid hormone quartiles using logistic regression models, adjusted for potential confounders.
Results Of the study patients, 12% (
n =1,664) had MetS. A higher T3 level and T3-to-T4 ratio were associated with unfavourable metabolic profiles, such as higher body mass index, systolic and diastolic blood pressure, triglycerides, fasting glucose and glycated hemoglobin, and lower high density lipoprotein cholesterol levels. The proportion of participants with MetS increased across the T3 quartile categories (P for trend <0.001) and the T3-to-T4 ratio quartile categories (P for trend <0.001). The multi-variate-adjusted OR (95% confidence interval) for MetS in the highest T3 quartile group was 1.249 (1.020 to 1.529) compared to the lowest T3 quartile group, and that in the highest T3-to-T4 ratio quartile group was 1.458 (1.141 to 1.863) compared to the lowest T3-to-T4 ratio quartile group, even after adjustment for potential confounders.Conclusion Serum T3 levels and T3-to-T4 ratio are independently associated with MetS in euthyroid middle-aged subjects. Longitudinal studies are needed to define this association and its potential health implications.
-
Citations
Citations to this article as recorded by- The effect of endocrine disrupting chemicals on the vitronectin-receptor (integrin αvβ3)-mediated cell adhesion of human umbilical vein endothelial cells
Maša Kenda, Urša Pečar Fonović, Janko Kos, Marija Sollner Dolenc
Toxicology in Vitro.2022; 79: 105275. CrossRef - Could the ketogenic diet induce a shift in thyroid function and support a metabolic advantage in healthy participants? A pilot randomized-controlled-crossover trial
Stella Iacovides, Shane K. Maloney, Sindeep Bhana, Zareena Angamia, Rebecca M. Meiring, Carla Pegoraro
PLOS ONE.2022; 17(6): e0269440. CrossRef - Mediation effects of thyroid function in the associations between phthalate exposure and lipid metabolism in adults
Han-Bin Huang, Po-Keng Cheng, Chi-Ying Siao, Yuan-Ting C. Lo, Wei-Chun Chou, Po-Chin Huang
Environmental Health.2022;[Epub] CrossRef - Cholinesterase homozygous genotype as susceptible biomarker of hypertriglyceridaemia for pesticide-exposed agricultural workers
Xingfan Zhou, Min Zhang, Yuqian Wang, Hailing Xia, Lijin Zhu, Guangyi Li, Li Rong, Huahuang Dong, Rui Chen, Shichuan Tang, Min Yu
Biomarkers.2021; 26(4): 335. CrossRef - Association between thyroid hormone and components of metabolic syndrome in euthyroid Korean adults
Kyung A. Shin, Eun Jae Kim
Medicine.2021; 100(51): e28409. CrossRef - Clinical Parameters Are More Likely to Be Associated with Thyroid Hormone Levels than with Thyrotropin Levels: A Systematic Review and Meta-Analysis
Stephen P. Fitzgerald, Nigel G. Bean, Henrik Falhammar, Jono Tuke
Thyroid.2020; 30(12): 1695. CrossRef - The role of thyroid hormone in metabolism and metabolic syndrome
Patrícia de Fátima dos Santos Teixeira, Patrícia Borges dos Santos, Carmen Cabanelas Pazos-Moura
Therapeutic Advances in Endocrinology and Metabolism.2020; 11: 204201882091786. CrossRef - Association between Abdominal Fat Distribution and Free Triiodothyronine in a Euthyroid Population
Xiaomin Nie, Yiting Xu, Xiaojing Ma, Yunfeng Xiao, Yufei Wang, Yuqian Bao
Obesity Facts.2020; 13(3): 358. CrossRef - Association of thyroid function with white coat hypertension and sustained hypertension
Peng Cai, Yan Peng, YuXi Chen, Li Li, Wei Chu, Yan Wang, Xukai Wang
The Journal of Clinical Hypertension.2019; 21(5): 674. CrossRef - Thyroid function is associated with body mass index and fasting plasma glucose in Thai euthyroid population
Amornpan Lertrit, La-or Chailurkit, Boonsong Ongphiphadhanakul, Wichai Aekplakorn, Chutintorn Sriphrapradang
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 468. CrossRef - Thyroid disease and the metabolic syndrome
Ladan Mehran, Atieh Amouzegar, Fereidoun Azizi
Current Opinion in Endocrinology, Diabetes & Obesity.2019; 26(5): 256. CrossRef - Morbid obez hastalarda kilo kaybının insulin direnci, bazal metabolizma hızı, antropometrik ölçümler ve tiroid fonksiyonlarına etkisi
Şenay DURMAZ CEYLAN, Şuuri Ahsen CEYLAN, Fatih EKER, Aşkın GÜNGÜNEŞ
Anadolu Güncel Tıp Dergisi.2019; 1(4): 99. CrossRef - Body Composition, Resting Energy Expenditure, and Metabolic Changes in Women Diagnosed with Differentiated Thyroid Carcinoma
Elena Izkhakov, Nachum Vaisman, Sophie Barnes, Micha Barchana, Naftali Stern, Lital Keinan-Boker
Thyroid.2019; 29(8): 1044. CrossRef - High TSH Level within Normal Range Is Associated with Obesity, Dyslipidemia, Hypertension, Inflammation, Hypercoagulability, and the Metabolic Syndrome: A Novel Cardiometabolic Marker
Yi-Cheng Chang, Shih-Che Hua, Chia-Hsuin Chang, Wei-Yi Kao, Hsiao-Lin Lee, Lee-Ming Chuang, Yen-Tsung Huang, Mei-Shu Lai
Journal of Clinical Medicine.2019; 8(6): 817. CrossRef - Metabolic Syndrome, Thyroid Function and Autoimmunity - The PORMETS Study
Luís Raposo, Sandra Martins, Daniela Ferreira, João Tiago Guimarães, Ana Cristina Santos
Endocrine, Metabolic & Immune Disorders - Drug Targets.2019; 19(1): 75. CrossRef - Hormesis in Health and Chronic Diseases
Xin Li, Tingting Yang, Zheng Sun
Trends in Endocrinology & Metabolism.2019; 30(12): 944. CrossRef - Relationship of metabolic syndrome and its components with thyroid dysfunction in Algerian patients
Mohamed Larbi Hamlaoui, Ammar Ayachi, Aoulia Dekaken, Adel Gouri
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2018; 12(1): 1. CrossRef - High free triiodothyronine and free-triiodothyronine-to-free-thyroxine ratio levels are associated with metabolic syndrome in a euthyroid population
Diego Urrunaga-Pastor, Mirella Guarnizo-Poma, Enrique Moncada-Mapelli, Luis G. Aguirre, Herbert Lazaro-Alcantara, Socorro Paico-Palacios, Betzi Pantoja-Torres, Vicente A. Benites-Zapata
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2018; 12(2): 155. CrossRef - Exploring the association between thyroid- stimulating hormone and metabolic syndrome: A large population-based study
Yi-Chao Zhou, Wen-Hui Fang, Tung-Wei Kao, Chung-Ching Wang, Yaw-Wen Chang, Tao-Chun Peng, Chen-Jung Wu, Hui-Fang Yang, James Yi-Hsin Chan, Wei-Liang Chen, Tatsuo Shimosawa
PLOS ONE.2018; 13(6): e0199209. CrossRef - Thyroid function and metabolic syndrome in the population-based LifeLines cohort study
Bruce H. R. Wolffenbuttel, Hanneke J. C. M. Wouters, Sandra N. Slagter, Robert P. van Waateringe, Anneke C. Muller Kobold, Jana V. van Vliet-Ostaptchouk, Thera P. Links, Melanie M. van der Klauw
BMC Endocrine Disorders.2017;[Epub] CrossRef - Hormetic effect of triiodothyronine in metabolically healthy obese persons
Ji Eun Jun, Tae Hyuk Kim, Seung-Eun Lee, You-Bin Lee, Jae Hwan Jee, Ji Cheol Bae, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Yong-Ki Min, Moon-Kyu Lee
Endocrine.2017; 57(3): 418. CrossRef - Association of triiodothyronine levels with future development of metabolic syndrome in euthyroid middle-aged subjects: a 6-year retrospective longitudinal study
Hye Jeong Kim, Ji Cheol Bae, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh, Myung Hi Yoo, Jee Jae Hwan, Jae Hyeon Kim, Yong-Ki Min, Sun Wook Kim, Jae Hoon Chung
European Journal of Endocrinology.2017; 176(4): 443. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- The effect of endocrine disrupting chemicals on the vitronectin-receptor (integrin αvβ3)-mediated cell adhesion of human umbilical vein endothelial cells

- Obesity and Metabolism
- Sex Factors in the Metabolic Syndrome as a Predictor of Cardiovascular Disease
- Sunghwan Suh, Jongha Baek, Ji Cheol Bae, Kyoung-Nyoun Kim, Mi Kyoung Park, Duk Kyu Kim, Nam H. Cho, Moon-Kyu Lee
- Endocrinol Metab. 2014;29(4):522-529. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.522
- 4,674 View
- 37 Download
- 16 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Metabolic syndrome (MetS) is a condition characterized by a cluster of metabolic disorders and is associated with increased risk of cardiovascular disease (CVD). This study analyzed data from the Korean Health and Genome Study to examine the impact of MetS on CVD.
Methods A total of 8,898 subjects (4,241 males and 4,657 females), 40 to 69 years of age, were enrolled and evaluated for the development of new onset CVD from 2001 to 2012 (median 8.1 years of follow-up).
Results The prevalence of MetS at baseline was 22.0% (932/4,241) and 29.7% (1,383/4,657) in males and females, respectively. MetS was associated with increased risk of coronary heart disease (CHD; hazard ratio [HR], 1.818; 95% confidence interval [CI], 1.312 to 2.520 in males; HR, 1.789; 95% CI, 1.332 to 2.404 in females) and CVD (HR, 1.689; 95% CI, 1.295 to 2.204 in males; HR, 1.686; 95% CI, 1.007 to 2.192 in females). Specifically, MetS was associated with risk of future stroke in females only (HR, 1.486; 95% CI, 1.007 to 2.192). Among MetS components, abdominal obesity and hypertension were independent predictors of both CHD and CVD. In addition, a higher number of MetS components correlated with higher CVD risk.
Conclusion MetS is a significant risk factor for the development of CVD although its impact varies between sexes.
-
Citations
Citations to this article as recorded by- Cardiovascular age of workers with different employment categories
Byung-Kook Lee, Jaeouk Ahn, Nam-Soo Kim, Jungsun Park, Yangho Kim
Archives of Environmental & Occupational Health.2022; 77(3): 243. CrossRef - Effects of Anthocyanin-rich Berries on the Risk of Metabolic Syndrome: A Systematic Review and Meta-analysis
Mikkel Roulund Wilken, Max Norman Tandrup Lambert, Christine Bodelund Christensen, Per Bendix Jeppesen
Review of Diabetic Studies.2022; 18(1): 42. CrossRef - Rate and risk factors of metabolic components and component combinations according to hypertension status in Tibetans in a cross-sectional study
Jihong Hu, Brian Thompson, Shuxia Wang, Minhao Guo, Chunjuan Yan, Fengfeng Ding, Peng Guo, Li Chen, Zhuoma Cao, Jianzong Wang
Medicine.2022; 101(43): e31320. CrossRef - Gender differences in changes in metabolic syndrome status and its components and risk of cardiovascular disease: a longitudinal cohort study
Azra Ramezankhani, Fereidoun Azizi, Farzad Hadaegh
Cardiovascular Diabetology.2022;[Epub] CrossRef - The Association of Metabolic Syndrome with the development of cardiovascular disease among Kazakhs in remote rural areas of Xinjiang, China: a cohort study
Wenwen Yang, Shuxia Guo, Haixia Wang, Yu Li, Xianghui Zhang, Yunhua Hu, Heng Guo, Kui Wang, Yizhong Yan, Jingyu Zhang, Jiaolong Ma, Lei Mao, Lati Mu, Jiaming Liu, Yanpeng Song, Changjing Li, Zhuo Ma, Rulin Ma, Jia He
BMC Public Health.2021;[Epub] CrossRef - Serum Arylsulfatase and Acid Phosphatase Activity in Patients with Metabolic Syndrome as a Result of Oxidative Damage to Lysosomes
Dorota M. Olszewska-Słonina
Protein & Peptide Letters.2021; 28(11): 1246. CrossRef - Validation of Risk Prediction Models for Atherosclerotic Cardiovascular Disease in a Prospective Korean Community-Based Cohort
Jae Hyun Bae, Min Kyong Moon, Sohee Oh, Bo Kyung Koo, Nam Han Cho, Moon-Kyu Lee
Diabetes & Metabolism Journal.2020; 44(3): 458. CrossRef - The Prevalence of Obesity and Metabolic Syndrome in the Korean Military Compared with the General Population
Jung Hwan Lee, Da Hea Seo, Min Jung Nam, Geon Hui Lee, Dong Hee Yang, Min Joo Lee, Ung-Rim Choi, Seongbin Hong
Journal of Korean Medical Science.2018;[Epub] CrossRef - Relationship between serum bilirubin levels and cardiovascular disease
Sunghwan Suh, Young Rak Cho, Mi Kyoung Park, Duk Kyu Kim, Nam H. Cho, Moon-Kyu Lee, Christian Herder
PLOS ONE.2018; 13(2): e0193041. CrossRef - Comparison Between Metabolic Syndrome and the Framingham Risk Score as Predictors of Cardiovascular Diseases Among Kazakhs in Xinjiang
Wenwen Yang, Rulin Ma, Xianghui Zhang, Heng Guo, Jia He, Lei Mao, Lati Mu, Yunhua Hu, Yizhong Yan, Jiaming Liu, Jiaolong Ma, Shugang Li, Yusong Ding, Mei Zhang, Jingyu Zhang, Shuxia Guo
Scientific Reports.2018;[Epub] CrossRef - Impact of interactions among metabolic syndrome components on the development of cardiovascular disease among Kazakhs in Xinjiang
Wenwen Yang, Xiang Gao, Xianghui Zhang, Yunhua Hu, Heng Guo, Kui Wang, Yizhong Yan, Jia He, Jingyu Zhang, Jiaolong Ma, Lei Mao, Lati Mu, Jiaming Liu, Shugang Li, Yusong Ding, Mei Zhang, Rulin Ma, Shuxia Guo, Mahesh Narayan
PLOS ONE.2018; 13(10): e0205703. CrossRef - Prediction of cardiovascular disease in Korean population: based on health risk appraisal of national health screening program
Jae Moon Yun, Tae Gon Yoo, Seung-Won Oh, Be Long Cho, Eunyoung Kim, Insob Hwang
Journal of the Korean Medical Association.2017; 60(9): 746. CrossRef - Metabolic Syndrome Is a Strong Risk Factor for Minor Ischemic Stroke and Subsequent Vascular Events
Guang-Sheng Wang, Dao-Ming Tong, Xiao-Dong Chen, Tong-Hui Yang, Ye-Ting Zhou, Xiao-Bo Ma, Gianpaolo Reboldi
PLOS ONE.2016; 11(8): e0156243. CrossRef - Metabolic syndrome related to cardiovascular events in a 10-year prospective study
Laura Kazlauskienė, Jūratė Butnorienė, Antanas Norkus
Diabetology & Metabolic Syndrome.2015;[Epub] CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Impact of Cadmium Exposure on the Association between Lipopolysaccharide and Metabolic Syndrome
Seung Han, Kyoung Ha, Ja Jeon, Hae Kim, Kwan Lee, Dae Kim
International Journal of Environmental Research and Public Health.2015; 12(9): 11396. CrossRef - Heat Killed Lactobacillus reuteri GMNL-263 Reduces Fibrosis Effects on the Liver and Heart in High Fat Diet-Hamsters via TGF-β Suppression
Wei-Jen Ting, Wei-Wen Kuo, Dennis Hsieh, Yu-Lan Yeh, Cecilia-Hsuan Day, Ya-Hui Chen, Ray-Jade Chen, Viswanadha Padma, Yi-Hsing Chen, Chih-Yang Huang
International Journal of Molecular Sciences.2015; 16(10): 25881. CrossRef
- Cardiovascular age of workers with different employment categories

- Adrenal gland
- Clinical Characteristics, Management, and Outcome of 22 Cases of Primary Hypophysitis
- Sun Mi Park, Ji Cheol Bae, Ji Young Joung, Yoon Young Cho, Tae Hun Kim, Sang-Man Jin, Sunghwan Suh, Kyu Yeon Hur, Kwang-Won Kim
- Endocrinol Metab. 2014;29(4):470-478. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.470
- 4,240 View
- 41 Download
- 26 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Primary hypophysitis causes varying degrees of endocrine dysfunction and mass effect. The natural course and best treatment have not been well established.
Methods Medical records of 22 patients who had been diagnosed with primary hypophysitis between January 2001 and March 2013 were retrospectively reviewed. Based on the anatomical location, we classified the cases as adenohypophysitis (AH), infundibuloneurohypophysitis (INH), and panhypophysitis (PH). Clinical presentation, endocrine function, pathologic findings, magnetic resonance imaging findings, and treatment courses were reviewed.
Results Among 22 patients with primary hypophysitis, 81.8% (18/22) had involvement of the posterior pituitary lobe. Two patients of the AH (2/3, 66.6%) and three patients of the PH (3/10, 30%) groups initially underwent surgical mass reduction. Five patients, including three of the PH (3/10, 33.3%) group and one from each of the AH (1/3, 33.3%) and INH (1/9, 11.1%) groups, initially received high-dose glucocorticoid treatment. Nearly all of the patients treated with surgery or high-dose steroid treatment (9/11, 82%) required continuous hormone replacement during the follow-up period. Twelve patients received no treatment for mass reduction due to the absence of acute symptoms and signs related to a compressive mass effect. Most of them (11/12, 92%) did not show disease progression, and three patients recovered partially from hormone deficiency.
Conclusion Deficits of the posterior pituitary were the most common features in our cases of primary hypophysitis. Pituitary endocrine defects responded less favorably to glucocorticoid treatment and surgery. In the absence of symptoms related to mass effect and with the mild defect of endocrine function, it may not require treatment to reduce mass except hormone replacement.
-
Citations
Citations to this article as recorded by- Secondary xanthogranulomatous hypophysitis mimicking a pituitary macroadenoma: a case report
Salma Salhi, Ibtissem Oueslati, Yasmine Mouelhi, Alia Zehani, Nidhameddine Kchir, Elyes Kamoun, Meriem Yazidi, Melika Chihaoui
Journal of International Medical Research.2024;[Epub] CrossRef - Glucocorticoid therapy as first-line treatment in primary hypophysitis: a systematic review and individual patient data meta-analysis
Brijesh Krishnappa, Ravikumar Shah, Saba Samad Memon, Chakra Diwaker, Anurag R Lila, Virendra A Patil, Nalini S Shah, Tushar R Bandgar
Endocrine Connections.2023;[Epub] CrossRef - Hypophysitis, the Growing Spectrum of a Rare Pituitary Disease
Fabienne Langlois, Elena V Varlamov, Maria Fleseriu
The Journal of Clinical Endocrinology & Metabolism.2022; 107(1): 10. CrossRef - Outcomes of Initial Management Strategies in Patients With Autoimmune Lymphocytic Hypophysitis: A Systematic Review and Meta-analysis
Diane Donegan, Zeb Saeed, Danae A Delivanis, Mohammad Hassan Murad, Juergen Honegger, Felix Amereller, Seda Hanife Oguz, Dana Erickson, Irina Bancos
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): 1170. CrossRef - Early Pulse Glucocorticoid Therapy and Improved Hormonal Outcomes in Primary Hypophysitis
Brijesh Krishnappa, Ravikumar Shah, Vijaya Sarathi, Anurag Ranjan Lila, Manjeet Kaur Sehemby, Virendra A. Patil, Shilpa Sankhe, Nalini Shah, Tushar Bandgar
Neuroendocrinology.2022; 112(2): 186. CrossRef - Preoperative differentiation of hypophysitis and pituitary adenomas using a novel clinicoradiologic scoring system
Kyla Wright, Hyon Kim, Travis Hill, Matthew Lee, Cordelia Orillac, Nikita Mogar, Donato Pacione, Nidhi Agrawal
Pituitary.2022; 25(4): 602. CrossRef - Hypophysitis
Diane Donegan, Jürgen Honegger
Endocrine Practice.2022; 28(9): 901. CrossRef - Rare Case of a Disappearing Pituitary Adenoma During the Coronavirus Disease 2019 (COVID-19) Pandemic
David P. Bray, C. Arturo Solares, Nelson M. Oyesiku
World Neurosurgery.2021; 146: 148. CrossRef - Diabetes insipidus secondary to sellar/parasellar lesions
Anna Angelousi, Chrysoula Mytareli, Paraskevi Xekouki, Eva Kassi, Konstantinos Barkas, Ashley Grossman, Gregory Kaltsas
Journal of Neuroendocrinology.2021;[Epub] CrossRef - Clinical presentation and management of hypophysitis: An observational study of case series
Marouan Karrou, Salma Benyakhlef, Achwak Alla, Najoua Messaoudi, Asmae Oulad Amar, Siham Rouf, Imane Kamaoui, Noureddine Oulali, Faycal Moufid, Naima Abda, Hanane Latrech
Surgical Neurology International.2021; 12: 304. CrossRef - Clinical aspects of autoimmune hypothalamitis, a variant of autoimmune hypophysitis: Experience from one center
Qian Wei, Guoqing Yang, Zhaohui Lue, Jingtao Dou, Li Zang, Yijun Li, Jin Du, Weijun Gu, Yiming Mu
Journal of International Medical Research.2020; 48(3): 030006051988783. CrossRef - Primary and Ipilimumab-induced Hypophysitis: A Single-center Case Series
Paul Atkins, Ehud Ur
Endocrine Research.2020; 45(4): 246. CrossRef - Hypophysitis (Including IgG4 and Immunotherapy)
Anna Angelousi, Krystallenia Alexandraki, Marina Tsoli, Gregory Kaltsas, Eva Kassi
Neuroendocrinology.2020; 110(9-10): 822. CrossRef - Hypophysitis in the era of immune checkpoint inhibitors and immunoglobulin G4-related disease
Leen Wehbeh, Sama Alreddawi, Roberto Salvatori
Expert Review of Endocrinology & Metabolism.2019; 14(3): 167. CrossRef - Immune check point inhibitors-induced hypophysitis: a retrospective analysis of the French Pharmacovigilance database
Julie Garon-Czmil, Nadine Petitpain, Franck Rouby, Marion Sassier, Samy Babai, Mélissa Yéléhé-Okouma, Georges Weryha, Marc Klein, Pierre Gillet
Scientific Reports.2019;[Epub] CrossRef - Clinical Features, Magnetic Resonance Imaging, and Treatment Experience of 20 Patients with Lymphocytic Hypophysitis in a Single Center
Qiang Zhu, Ke Qian, Guijun Jia, Gang Lv, Jisheng Wang, Liyong Zhong, Shuqing Yu
World Neurosurgery.2019; 127: e22. CrossRef - Idiopathic granulomatous hypophysitis presenting with galactorrhea, headache, and nausea in a woman: a case report and review of the literature
Guive Sharifi, Mohammad Reza Mohajeri-Tehrani, Behrouz Navabakhsh, Bagher Larijani, Touraj Valeh
Journal of Medical Case Reports.2019;[Epub] CrossRef - Paciente de 31 años con polidipsia
A.R. Benavides Aramburu, M. Seguí Díaz
Medicina de Familia. SEMERGEN.2018; 44(2): e77. CrossRef - Primary hypophysitis and other autoimmune disorders of the sellar and suprasellar regions
Sriram Gubbi, Fady Hannah-Shmouni, Constantine A. Stratakis, Christian A. Koch
Reviews in Endocrine and Metabolic Disorders.2018; 19(4): 335. CrossRef - Primary lymphocytic hypophysitis: Clinical characteristics and treatment of 50 cases in a single centre in China over 18 years
Shuchang Wang, Linjie Wang, Yong Yao, Feng Feng, Hongbo Yang, Zhiyong Liang, Kan Deng, Hui You, Jian Sun, Bing Xing, Zimeng Jin, Renzhi Wang, Hui Pan, Huijuan Zhu
Clinical Endocrinology.2017; 87(2): 177. CrossRef - Clinical presentation and outcome of children with central diabetes insipidus associated with a self‐limited or transient pituitary stalk thickening, diagnosed as infundibuloneurohypophysitis
J. Schaefers, M. Cools, K. De Waele, I. Gies, V. Beauloye, P. Lysy, I. Francois, D. Beckers, J. De Schepper
Clinical Endocrinology.2017; 87(2): 171. CrossRef - Intrachiasmatic abscess caused by IgG4-related hypophysitis
Georgios F. Hadjigeorgiou, Eva Løbner Lund, Lars Poulsgaard, Ulla Feldt-Rasmussen, Åse Krogh Rasmussen, Marianne Wegener, Kåre Fugleholm
Acta Neurochirurgica.2017; 159(11): 2229. CrossRef - Granulomatous and lymphocytic hypophysitis – are they immunologically distinct?
Shilpa Rao, Anita Mahadevan, Tanmoy Maiti, Manish Ranjan, Shivayogi Durgad Shwetha, Arimappamagan Arivazhagan, Jitender Saini
APMIS.2016; 124(12): 1072. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Secondary xanthogranulomatous hypophysitis mimicking a pituitary macroadenoma: a case report

- Adrenal gland
- Subclinical Cushing's Syndrome and Metabolic Disorder
- Ji Cheol Bae
- Endocrinol Metab. 2014;29(4):441-442. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.441
- 2,779 View
- 32 Download

- Thyroid
- Steroid Responsive Xanthomatous Hypophysitis Associated with Autoimmune Thyroiditis: A Case Report
- Ji Young Joung, Hyemin Jeong, Yoon Young Cho, Kyoungmin Huh, Yeon-Lim Suh, Kwang-Won Kim, Ji Cheol Bae
- Endocrinol Metab. 2013;28(1):65-69. Published online March 25, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.1.65
- 3,478 View
- 30 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader We report the case of a 36-year-old woman who presented with headache, fever, and amenorrhea. Laboratory analysis revealed hypopituitarism and autoimmune thyroiditis, while a cerebrospinal fluid study suggested concurrent aseptic meningitis. A magnetic resonance image (MRI) scan revealed a 1.0×0.9 cm cystic mass enlarging the sella turcica. Surgical resection via an endoscopic transsphenoidal route was performed. The histological finding of the excised tissue revealed foamy histiocytes with vacuolated cytoplasm, supporting the diagnosis of xanthomatous hypophysitis. Although a residual soft lesion was observed on the MRI image postoperatively, the patient's headache and fever improved. Ten months after surgery, the patient complained of visual impairment and headache, and the residual mass had enlarged into the suprasellar area. High dose (500 mg intravenous) methylprednisolone was administered for 3 days. During the methylprednisolone pulse therapy, the patient's visual acuity and headache improved. A follow-up MRI taken after methylprednisolone therapy showed a marked mass reduction. Our case supports an autoimmune pathophysiology for xanthomatous hypophysitis and suggests that high dose glucocorticoid therapy as a treatment option.
-
Citations
Citations to this article as recorded by- Xanthomatous hypophysitis causing hypogonadotropic hypogonadism resulting in delayed presentation of slipped capital femoral epiphysis
Kirit Singh, Avinash Kumar Kanodia, Peter Ross, Antonia Torgersen, Jamie Maclean, Graham Leese, Kismet Hossain-Ibrahim
British Journal of Neurosurgery.2022; 36(2): 286. CrossRef - Full recovery from chronic headache and hypopituitarism caused by lymphocytic hypophysitis: A case report
Mao-Guang Yang, Han-Qing Cai, Si-Si Wang, Lin Liu, Chun-Mei Wang
World Journal of Clinical Cases.2022; 10(3): 1041. CrossRef - Xanthomatous Hypophysitis Secondary to a Ruptured Rathke’s Cleft Cyst: A Case Report
Emre Gezer, Burak Çabuk, Büşra Yaprak Bayrak, Zeynep Cantürk, Berrin Çetinarslan, Alev Selek, Mehmet Sözen, Damla Köksalan, Savaş Ceylan
Brain Tumor Research and Treatment.2022; 10(1): 48. CrossRef - Successful immunomodulatory treatment for recurrent xanthogranulomatous hypophysitis in an adolescent: illustrative case
Sarah DeCou, Pablo F. Recinos, Richard A. Prayson, Christopher Karakasis, Anzar Haider, Neha Patel
Journal of Neurosurgery: Case Lessons.2022;[Epub] CrossRef - Xanthogranulomatous hypophysitis: A rare presentation in a young female patient
Mohammad Ali Yaghoubi, Samira Zabihyan, Amin Saeidinia, Masoumeh Gharib, Ramin Ghiyasi Moghaddam
Clinical Case Reports.2022;[Epub] CrossRef - Xanthomatous Hypophysitis Presenting in an Adolescent Girl: A Long-Term Follow-Up of a Rare Case and Review of the Literature
Jeanne Sze Lyn Wong, Azraai Bahari Nasruddin, Nalini M. Selveindran, Kartikasalwah Abd Latif, Fauziah Kassim, Sukanya Banerjee Nair, Janet Y.H. Hong
AACE Clinical Case Reports.2021; 7(3): 220. CrossRef - Xanthomatous Hypophysitis: A Case Report and Comprehensive Literature Review
Jianyu Zhu, Zhicheng Wang, Wenze Wang, Jinghua Fan, Yi Zhang, Xiaoxu Li, Jie Liu, Shenzhong Jiang, Kan Deng, Lian Duan, Yong Yao, Huijuan Zhu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Recurring Primary Xanthomatous Hypophysitis Behaving Like Pituitary Adenoma: Additional Case and Literature Review
Mansour Mathkour, Tyler Zeoli, Cassidy Werner, Tyler Scullen, Juanita Garces, Joseph Keen, Marcus Ware
World Neurosurgery.2020; 138: 27. CrossRef - Imaging findings in hypophysitis: a review
Ferdinando Caranci, Giuseppe Leone, Andrea Ponsiglione, Massimo Muto, Fabio Tortora, Mario Muto, Sossio Cirillo, Luca Brunese, Alfonso Cerase
La radiologia medica.2020; 125(3): 319. CrossRef - Hypophysitis in the era of immune checkpoint inhibitors and immunoglobulin G4-related disease
Leen Wehbeh, Sama Alreddawi, Roberto Salvatori
Expert Review of Endocrinology & Metabolism.2019; 14(3): 167. CrossRef - Xanthomatous Hypophysitis Is Associated with Ruptured Rathke’s Cleft Cyst
Kai Duan, Sylvia L. Asa, Daniel Winer, Zadeh Gelareh, Fred Gentili, Ozgur Mete
Endocrine Pathology.2017; 28(1): 83. CrossRef - Xanthomatous Hypophysitis Presenting with Diabetes Insipidus Completely Cured Through Transsphenoidal Surgery: Case Report and Literature Review
Wei Lin, Lu Gao, Xiaopeng Guo, Wenze Wang, Bing Xing
World Neurosurgery.2017; 104: 1051.e7. CrossRef - Review of xanthomatous lesions of the sella
B.K. Kleinschmidt‐DeMasters, Kevin O. Lillehei, Todd C. Hankinson
Brain Pathology.2017; 27(3): 377. CrossRef - Xanthomatous hypophysitis
Bishoy Hanna, Yan M. Li, Timothy Beutler, Parul Goyal, Walter A. Hall
Journal of Clinical Neuroscience.2015; 22(7): 1091. CrossRef - Clinical Characteristics, Management, and Outcome of 22 Cases of Primary Hypophysitis
Sun Mi Park, Ji Cheol Bae, Ji Young Joung, Yoon Young Cho, Tae Hun Kim, Sang-Man Jin, Sunghwan Suh, Kyu Yeon Hur, Kwang-Won Kim
Endocrinology and Metabolism.2014; 29(4): 470. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Xanthomatous hypophysitis causing hypogonadotropic hypogonadism resulting in delayed presentation of slipped capital femoral epiphysis

- Obesity and Metabolism
- Association between Serum Albumin, Insulin Resistance, and Incident Diabetes in Nondiabetic Subjects
- Ji Cheol Bae, Sung Hwan Seo, Kyu Yeon Hur, Jae Hyeon Kim, Myung-Shik Lee, Moon Kyu Lee, Won Young Lee, Eun Jung Rhee, Ki Won Oh
- Endocrinol Metab. 2013;28(1):26-32. Published online March 25, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.1.26
- 4,591 View
- 42 Download
- 36 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Serum albumin has been suggested to be associated with insulin resistance. We evaluated the association between serum albumin concentration and insulin resistance. We also investigated whether serum albumin level has an independent effect on the development of diabetes.
Methods In our study, 9,029 subjects without diabetes, who underwent comprehensive health check-ups annually for 5 years, were categorized into tertiles based on their serum albumin levels at baseline. The odds ratio (OR) for the prevalence of insulin resistance, defined as the top quartile of homeostasis model assessment of insulin resistance and the presence of impaired fasting glucose and nonalcoholic fatty liver disease, was evaluated cross-sectionally. Also, the hazard ratio (HR) for incident diabetes was estimated longitudinally, according to the baseline albumin tertiles using Cox proportional hazard analysis respectively.
Results From the lowest to the highest tertile of albumin, the multivariable-adjusted ORs of insulin resistance increased significantly in both men and women. During the mean follow-up period of nearly 4 years, 556 (6.1%) subjects progressed to diabetes. The multivariable-adjusted HR (95% confidence interval [CI]) of diabetes in men were 1, 1.09 (95% CI, 0.86 to 1.40), and 1.10 (95% CI, 0.86 to 1.41), respectively, from the lowest to the highest tertiles of baseline albumin. Corresponding values for women were 1, 1.21 (95% CI, 0.66 to 2.21), and 1.06 (95% CI, 0.56 to 2.02), respectively.
Conclusion Our study showed that increased serum albumin level was associated with insulin resistance. However, serum albumin did not have an independent effect on the development of diabetes.
-
Citations
Citations to this article as recorded by- Prevalence of Non-alcoholic Fatty Liver Disease Detected by Computed Tomography in the General Population Compared with Ultrasonography
Yuki Ito, Kentaro Yoshioka, Kazuhiko Hayashi, Yuko Shimizu, Ryo Fujimoto, Ryosuke Yamane, Michiyo Yoshizaki, Go Kajikawa, Taro Mizutani, Hidemi Goto
Internal Medicine.2024; 63(2): 159. CrossRef - Geriatric nutritional risk index is correlated with islet function but not insulin resistance in elderly patients with type 2 diabetes: A retrospective study
Nan Geng, Yaxue Gao, Yuanyuan Ji, Yingchun Niu, Cuijuan Qi, Yunfeng Zhen, Jinhu Chen, Luping Ren
Medicine.2024; 103(11): e37438. CrossRef - Blood Urea Nitrogen to Serum Albumin Ratio as A New Prognostic
Indicator in Critically Ill Patients with Diabetic Ketoacidosis: A Retrospective
Cohort Study
Tingting Hang, Jing Huang, Guiping He, Jin Li, Tingting Tao
Experimental and Clinical Endocrinology & Diabetes.2024;[Epub] CrossRef - Sex difference in the associations among liver function parameters with incident diabetes mellitus in a large Taiwanese population follow-up study
Yi-Kong Chen, Pei-Yu Wu, Jiun-Chi Huang, Szu-Chia Chen, Jer-Ming Chang
Frontiers in Public Health.2023;[Epub] CrossRef - Antidiabetic Properties of Nymphaea Species (Water Lilies): A Review
A. H. M. Safayet Ullah Prodhan, Farzana Sharmin Mridu
The Natural Products Journal.2023;[Epub] CrossRef - Gestational diabetes in women living with HIV in the UK and Ireland: insights from population‐based surveillance data
Laurette L. Bukasa, Mario Cortina‐Borja, Helen Peters, Graham P. Taylor, Claire Thorne
Journal of the International AIDS Society.2023;[Epub] CrossRef - Cancer and Diabetes: Predictive Factors in Patients with Metabolic Syndrome
Mihai Cosmin Stan, Daniel Georgescu, Ciprian Camil Mireștean, Florinel Bădulescu
Diagnostics.2023; 13(16): 2647. CrossRef - Role of liver parameters in diabetes mellitus – a narrative review
Sana Rafaqat, Aqsa Sattar, Amber Khalid, Saira Rafaqat
Endocrine Regulations.2023; 57(1): 200. CrossRef - Differential cellular responses to FDA-approved nanomedicines: an exploration of albumin-based nanocarriers and liposomes in protein corona formation
Athika Darumas Putri, Ming-Jen Hsu, Chia-Li Han, Fang-Ching Chao, Chun-Hua Hsu, Christian D. Lorenz, Chien-Ming Hsieh
Nanoscale.2023; 15(44): 17825. CrossRef - Association of the HALP Score with Dyslipidemia: A Large, Nationwide Retrospective Study
Yazeed Alshuweishi, Ahmed M. Basudan, Mohammed Alfaifi, Hussam Daghistani, Mohammad A. Alfhili
Medicina.2023; 59(11): 2002. CrossRef - Preventive and Ameliorative Effects of Diet Supplemented with Cucurbita maxima Leaf on Hyperglycemia and Hepatotoxicity in STZ-Induced Diabetic Rats
Job Itanyi Onuche, Arowora Kayode Adebisi , Joseph Ikwebe, Michael Sunday Abu
Asian Journal of Biological Sciences.2023; 16(4): 502. CrossRef - Lower Plasma Albumin, Higher White Blood Cell Count and High-Sensitivity C-Reactive Protein are Associated with Femoral Artery Intima-Media Thickness Among Newly Diagnosed Patients with Type 2 Diabetes Mellitus
Nga Phi Thi Nguyen, Thuc Luong Cong, Thi Thanh Hoa Tran, Binh Nhu Do, Son Tien Nguyen, Binh Thanh Vu, Lan Ho Thi Nguyen, Manh Van Ngo, Hoa Trung Dinh, Hoang Duong Huy, Nghia Xuan Vu, Kien Nguyen Trung, Duong Ngoc Vu, Nghia The Pham, Tuan Dinh Le
International Journal of General Medicine.2022; Volume 15: 2715. CrossRef - Liver-function parameters are associated with incident hypertension in a large Taiwanese population follow-up study
Yi-Hsueh Liu, Szu-Chia Chen, Wen-Hsien Lee, Ying-Chih Chen, Jiun-Chi Huang, Pei-Yu Wu, Chih-Hsing Hung, Chao-Hung Kuo, Ho-Ming Su
Journal of Human Hypertension.2022; 37(6): 496. CrossRef - Can probiotic, prebiotic, and synbiotic supplementation modulate the gut-liver axis in type 2 diabetes? A narrative and systematic review of clinical trials
Yousef Al-Najjar, Maryam Arabi, Pradipta Paul, Ali Chaari
Frontiers in Nutrition.2022;[Epub] CrossRef - Albumin infusion ameliorates liver injury in streptozotocin-induced diabetic rats
CS Bae, T Ahn
Veterinární medicína.2022; 67(5): 245. CrossRef - Ameliorative effect of Annona reticulata L. leaf extract on antihyperglycemic activity and its hepato-renal protective potential in streptozotocin induced diabetic rats
Vineela Pulivarthi, Josthna P., C.V. Naidu
Journal of Ayurveda and Integrative Medicine.2021; 12(3): 415. CrossRef - MALDI-TOF MS Characterisation of the Serum Proteomic Profile in Insulin-Resistant Normal-Weight Individuals
Katarzyna Pastusiak, Eliza Matuszewska, Dagmara Pietkiewicz, Jan Matysiak, Pawel Bogdanski
Nutrients.2021; 13(11): 3853. CrossRef - Insulin sensitivity variations in apparently healthy Arab male subjects: correlation with insulin and C peptide
Noor Suleiman, Meis Alkasem, Shaimaa Hassoun, Ibrahem Abdalhakam, Ilham Bettahi, Fayaz Mir, Manjunath Ramanjaneya, Jayakumar Jerobin, Ahmad Iskandarani, Tareq A Samra, Prem Chandra, Monica Skarulis, Abdul Badi Abou-Samra
BMJ Open Diabetes Research & Care.2021; 9(2): e002039. CrossRef - U-shaped association between serum albumin and development of chronic kidney disease in general hypertensive patients
Chongfei Jiang, Binyan Wang, Youbao Li, Liling Xie, Xianglin Zhang, Jiancheng Wang, Yaren Yu, Yun Song, Min Liang, Guobao Wang, Jianping Li, Yan Zhang, Lishun Liu, Chengzhang Liu, Genfu Tang, Yong Huo, Xiping Xu, Xianhui Qin
Clinical Nutrition.2020; 39(1): 258. CrossRef - Serum albumin cysteine trioxidation is a potential oxidative stress biomarker of type 2 diabetes mellitus
Selvam Paramasivan, Sunil S. Adav, SoFong Cam Ngan, Rinkoo Dalan, Melvin Khee-Shing Leow, Hee Hwa Ho, Siu Kwan Sze
Scientific Reports.2020;[Epub] CrossRef - Serum albumin, cardiometabolic and other adverse outcomes: systematic review and meta-analyses of 48 published observational cohort studies involving 1,492,237 participants
Samuel Seidu, Setor K. Kunutsor, Kamlesh Khunti
Scandinavian Cardiovascular Journal.2020; 54(5): 280. CrossRef - Skeletal muscle reprogramming by breast cancer regardless of treatment history or tumor molecular subtype
Hannah E. Wilson, David A. Stanton, Cortney Montgomery, Aniello M. Infante, Matthew Taylor, Hannah Hazard-Jenkins, Elena N. Pugacheva, Emidio E. Pistilli
npj Breast Cancer.2020;[Epub] CrossRef - Prevalence of nutritional deficiencies in bariatric surgery candidates and its effect on metabolic status
Sílvia Cristina de Sousa Paredes, Fernando Mota-Garcia
Hormones.2020; 19(4): 505. CrossRef The Product of Red Blood Cells and Hematocrit Can Be Used as a Novel Indicator of Impaired Fasting Blood Glucose Status
Ling Feng, Haishan Chen, Jianhui Chen, Chongxiang Xiong, Xiaofei Shao, Xin Wang, Jing Ning, Zhicong Xiang, Xuan Wang, Tong Chen, Hua Xiao, Hongjuan Tang, Xiaolin Li, Guobao Hong, Hequn Zou
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4007. CrossRef- Thiol/Disulphide homeostasis, ischemia modified albumin, and ferroxidase as oxidative stress markers in women with obesity with insulin resistance
Elif Ates, Turan Set, Süleyman Caner Karahan, Cemile Biçer, Özcan Erel
Journal of Medical Biochemistry.2019; 38(4): 445. CrossRef - Insulin resistance and chronic kidney disease progression, cardiovascular events, and death: findings from the chronic renal insufficiency cohort study
Sarah J. Schrauben, Christopher Jepson, Jesse Y. Hsu, F. Perry Wilson, Xiaoming Zhang, James P. Lash, Bruce M. Robinson, Raymond R. Townsend, Jing Chen, Leon Fogelfeld, Patricia Kao, J. Richard Landis, Daniel J. Rader, L. Lee Hamm, Amanda H. Anderson, Har
BMC Nephrology.2019;[Epub] CrossRef - Association of Insulin Based Insulin Resistance with Liver Biomarkers in Type 2 Diabetes mellitus
Usha Adiga, Kathyayani P, Nandith P.B
Journal of Pure and Applied Microbiology.2019; 13(2): 1199. CrossRef - Establishment of an ex Vivo Model of Nonalcoholic Fatty Liver Disease Using a Tissue-Engineered Liver
Qiao Wu, Juan Liu, Lijin Liu, Yu Chen, Jie Wang, Ling Leng, Qunfang Yu, Zhongping Duan, Yunfang Wang
ACS Biomaterials Science & Engineering.2018; 4(8): 3016. CrossRef - Utility of Serum Albumin for Predicting Incident Metabolic Syndrome according to Hyperuricemia
You-Bin Lee, Ji Eun Jun, Seung-Eun Lee, Jiyeon Ahn, Gyuri Kim, Jae Hwan Jee, Ji Cheol Bae, Sang-Man Jin, Jae Hyeon Kim
Diabetes & Metabolism Journal.2018; 42(6): 529. CrossRef - Association of angiotensin-II levels with albuminuria in subjects with normal glucose metabolism, prediabetes, and type 2 diabetes mellitus
Se Hee Min, Sung Hye Kong, Jie-Eun Lee, Dong-Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Kyong Soo Park, Hak Chul Jang, Soo Lim
Journal of Diabetes and its Complications.2017; 31(10): 1499. CrossRef - Three-dimensional perfused human in vitro model of non-alcoholic fatty liver disease
Tomasz Kostrzewski, Terri Cornforth, Sophie A Snow, Larissa Ouro-Gnao, Cliff Rowe, Emma M Large, David J Hughes
World Journal of Gastroenterology.2017; 23(2): 204. CrossRef - Higher serum albumin was related with diabetes incidence and the impact of BMI changes: Based on cohort study of 18,384 Chinese male elderly
Miao Liu, Jingping Tang, Jing Zeng, Yao He
Journal of Diabetes and its Complications.2017; 31(12): 1663. CrossRef - HbA1c as a Screening tool for Ketosis in Patients with Type 2 Diabetes Mellitus
Bing Zhu, Le Bu, Manna Zhang, Aaron M. Gusdon, Liang Zheng, Sharvan Rampersad, Jue Li, Shen Qu
Scientific Reports.2016;[Epub] CrossRef - Association between Serum Albumin Concentration and Ketosis Risk in Hospitalized Individuals with Type 2 Diabetes Mellitus
Po-Chung Cheng, Shang-Ren Hsu, Yun-Chung Cheng
Journal of Diabetes Research.2016; 2016: 1. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef - Serum Albumin Levels: A Simple Answer to a Complex Problem? Are We on the Right Track of Assessing Metabolic Syndrome?
Sohee Kim, Shinae Kang
Endocrinology and Metabolism.2013; 28(1): 17. CrossRef
- Prevalence of Non-alcoholic Fatty Liver Disease Detected by Computed Tomography in the General Population Compared with Ultrasonography


 KES
KES

 First
First Prev
Prev



